Why Houston’s Asthma Specialists Are Turning to Clinical Trials for Better Outcomes
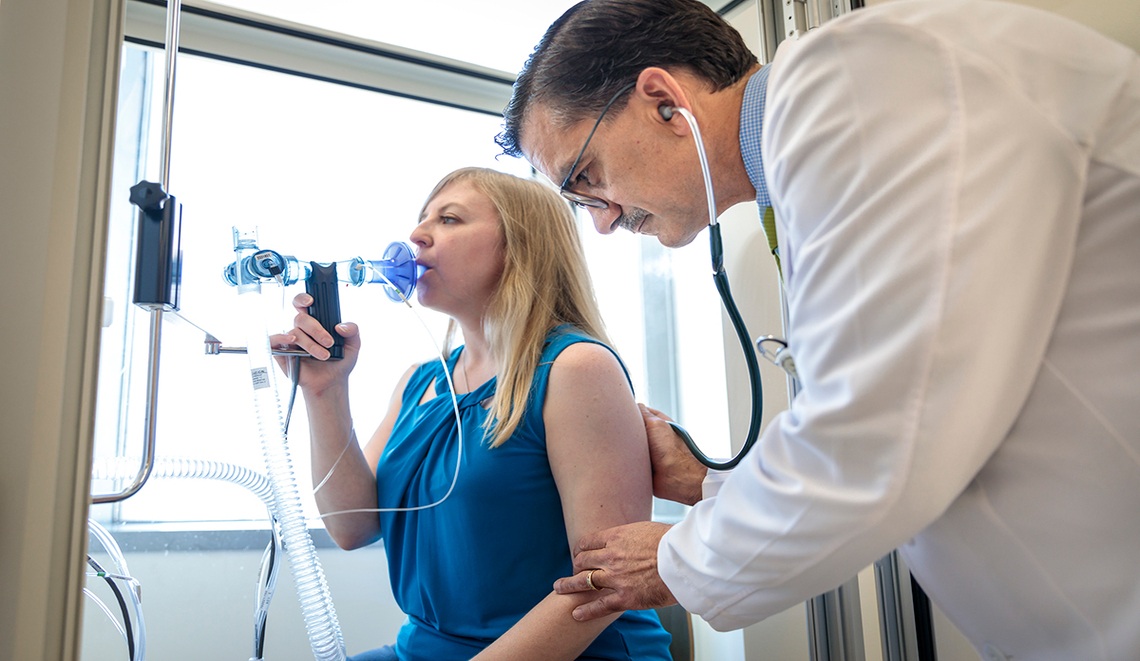
Introduction: Asking the Right QuestionEver wonder why, despite having inhalers, steroids and rescue meds widely available, so many patients with asthma still have such a tough time?Many people in Houston have to deal with this on a regular basis. Living with asthma may require you to miss work, experience severe allergy seasons or visit the emergency room (ER) when breathing becomes more difficult. Eventually, it makes many of us wonder: what else may be out there that could truly change things?Asthma in Texas: The Numbers Behind the ConcernAsthma is more common than many realize in Texas. Based on CDC data, about 7.3% of adults in Texas have asthma. That translates to over a million people managing the condition—for some, it's a daily reality, while for others, it's more seasonal.Here in Houston, our local environment can add another layer of challenge. Factors like high humidity, pollen levels, air quality, and even stormy weather can all contribute to making asthma more difficult to manage. That’s exactly why asthma specialists Houston here look past standard treatments for new options.The Ongoing Challenges in Asthma CareWhen Medications Aren’t EnoughFor most patients, asthma care means using inhaled steroids or bronchodilators. They help, but they’re not the complete solution. Some still face sudden flare-ups, others deal with unwanted side effects and many find it tough to stay on track with treatment over time.The Toll on Daily LifeIn reality, asthma is much more than just a cough or a wheeze. It can mean children missing school, parents constantly worrying about a late-night emergency and adults feeling held back from their daily lives at work and home. Even with standard care, quality of life often suffers. This is why specialists are paying more attention to another option which is clinical trials.Why Clinical Trials Matter in Asthma TreatmentWhat They ArePut simply, clinical trials are studies that test new treatments and approaches to care. The point is to find out: does it work better than today’s options, and can people use it safely? Who benefits most?Why Specialists Trust ThemIn Houston, specialists know how many modern asthma treatments began with clinical trials. Biologics, powerful drugs for severe asthma, were first offered only in research studies. For patients who’ve used all the common medicines, trials can give fresh hope supported by science.What Patients Can Gain from Clinical TrialsAccess to New Options EarlyTrials give patients the chance to try medications or therapies that may not reach the wider public for years. For those with severe asthma, this can mean fewer hospital visits and better control of symptoms.More Personalized CareMany clinical studies are built around precision medicine—treatments that match a patient’s own biology. This moves away from the one-plan-for-all model and gives patients care designed just for them.Helping Others TooJoining a trial helps more than one person. The results improve future care for children, families, and whole communities.Common Questions About Clinical Trials“Are they safe?”Yes. Clinical trials must meet strict standards and are closely monitored. Patients are fully informed of risks and benefits before deciding to join.“Who can join?”It varies by study. Some are aimed at adults, some at children. Certain trials are for people with severe asthma or those not helped by usual medicines. Doctors can guide patients to the right option.“Where do I find them in Houston?”Houston hosts well-known research centers. Clinical networks like Biopharma Informatic also connect patients with ongoing trials and volunteer chances.Why Houston Is Leading This EffortHouston’s diverse community and tough environment make it a key spot for asthma research. Doctors here see every day how treatments work differently for each patient, and they know better answers are needed. For them, clinical trials aren’t just numbers—they’re a way to raise the quality of care.ConclusionAsthma continues to affect daily life for many people in Houston. But clinical trials are helping bring fresh ideas and options. They let patients try new treatments early, get care that feels more personal, and join in the progress being made for asthma care.If you or someone in your life has asthma, it may be worth seeing what clinical trials in Houston have to offer. Biopharma Informatic provides information about ongoing studies and ways to volunteer. Every step in research brings us closer to a time when asthma is less disruptive—and breathing comes a little easier.